Soft food ideas after surgery are crucial for a smooth recovery. Following surgical procedures, your body needs easily digestible nourishment to heal. This guide provides essential insights into soft food diets, detailing why they’re easier on your system and the typical timelines for their implementation. We’ll explore various surgical scenarios where soft foods are recommended, from common procedures to the duration of the diet based on specific surgeries.
This comprehensive guide will cover everything from cooking methods and food choices to recipes, snack options, and hydration strategies. We’ll also delve into managing potential challenges like constipation, nausea, and loss of appetite, along with adapting recipes for dietary restrictions and ensuring food safety. Furthermore, we’ll address the emotional aspects of dietary changes, potential complications, and long-term dietary considerations for sustained well-being.
Introduction to Soft Food Diets After Surgery
Following surgical procedures, transitioning to a soft food diet is a critical component of the recovery process. This dietary approach aids in healing, minimizes digestive strain, and helps patients gradually return to a regular eating pattern. The specific guidelines and duration of the soft food diet can vary depending on the type of surgery performed and the individual’s recovery progress.Soft foods are generally easier to digest after surgery because they require less effort from the digestive system.
Surgical interventions can often lead to inflammation, swelling, and reduced digestive capacity. Soft foods minimize the workload on the gastrointestinal tract, reducing discomfort and allowing the body to focus its energy on healing. This is particularly important in the initial days and weeks after surgery.
Typical Timeframe for Soft Food Diets
The duration of a soft food diet varies considerably, based on the nature of the surgery and individual patient factors. Generally, the timeframe can range from a few days to several weeks.The following factors influence the duration:
- Type of Surgery: Procedures involving the gastrointestinal tract, such as bariatric surgery or bowel resections, typically necessitate a longer soft food phase. For example, after a gastric bypass, patients often start with a liquid diet, progressing to pureed foods, and eventually to soft foods over several weeks. Surgeries in other areas, such as oral surgery, may require a soft food diet until the surgical site heals sufficiently.
- Individual Healing Rate: Each patient’s recovery process is unique. Factors like age, overall health, and the presence of any underlying medical conditions can affect how quickly a person can tolerate solid foods.
- Post-operative Complications: The occurrence of complications, such as nausea, vomiting, or digestive issues, can prolong the soft food phase. If a patient experiences these issues, the healthcare team may recommend sticking to soft foods for a longer duration to avoid exacerbating symptoms.
- Healthcare Provider Recommendations: The surgeon or a registered dietitian will provide specific guidelines tailored to the individual’s needs and the surgical procedure. They will assess the patient’s progress and adjust the diet as needed.
In many cases, patients may gradually introduce solid foods back into their diet as their digestive system recovers. This process often involves starting with pureed foods, progressing to soft foods, and then slowly reintroducing solid foods. This incremental approach helps the body adjust to the changes in food texture and volume.
Types of Surgical Procedures Requiring Soft Food
A soft food diet is a critical component of recovery following various surgical procedures. The specific requirements and duration of this dietary adjustment vary depending on the type of surgery performed. This section Artikels common surgical procedures where a soft food diet is typically recommended, along with considerations for dietary duration.
Procedures Affecting the Digestive System
Surgical interventions within the digestive system often necessitate a soft food diet to minimize stress on the healing tissues and facilitate proper digestion.
- Esophageal Surgery: Procedures like esophagectomy (removal of part or all of the esophagus) or esophageal dilation (widening of a narrowed esophagus) often require a prolonged soft food diet. The duration can range from several weeks to months, depending on the complexity of the surgery and the patient’s healing progress. For example, following an esophagectomy, patients may initially consume only liquids, gradually progressing to pureed foods and then soft solids as tolerated.
- Gastric Surgery: Surgeries involving the stomach, such as gastrectomy (removal of part or all of the stomach) or bariatric procedures (e.g., gastric bypass, sleeve gastrectomy), mandate a soft food diet. In the initial post-operative phase, patients are typically limited to clear liquids, progressing to full liquids, pureed foods, and eventually soft solids. The transition and duration depend on the specific surgery and individual healing, but can span several weeks or even months.
- Intestinal Surgery: Surgeries on the small or large intestine, including bowel resections or procedures for conditions like Crohn’s disease or ulcerative colitis, also often require a soft food diet. The diet helps to reduce the workload on the digestive system and allow the intestines to heal. The length of time on a soft food diet varies based on the extent of the surgery and the individual’s recovery.
- Appendectomy: While a relatively minor procedure, a soft food diet may be recommended for a few days to a week after an appendectomy to allow the digestive system to recover and reduce the risk of complications.
Procedures Affecting the Mouth and Throat
Surgeries involving the mouth and throat inherently impact the ability to chew and swallow, thus necessitating a soft food diet.
- Tonsillectomy and Adenoidectomy: Following tonsillectomy (removal of the tonsils) and/or adenoidectomy (removal of the adenoids), a soft, non-irritating diet is crucial. Patients often begin with liquids and progress to soft foods like applesauce, yogurt, and mashed potatoes as tolerated. The duration is usually a week or two, until the throat has healed.
- Oral and Maxillofacial Surgery: Procedures such as jaw surgery, oral cancer surgery, or repair of facial fractures frequently require a soft or liquid diet for several weeks. This allows the surgical sites to heal without the stress of chewing. The specific diet and duration depend on the type of surgery and the extent of the procedures.
Other Surgical Procedures
Various other surgical procedures can necessitate a soft food diet as part of the recovery process.
- Head and Neck Cancer Surgery: Following surgery for head and neck cancers, a soft food diet is often necessary, particularly if the surgery involves the mouth, throat, or esophagus. The duration depends on the specific surgery and the patient’s ability to swallow and tolerate food.
- Dental Procedures: Certain dental procedures, such as extractions, implant placement, or jaw surgery, can require a soft food diet for a short period to allow the mouth to heal.
Variations in Diet Duration
The duration of a soft food diet varies significantly based on several factors. These include the type and complexity of the surgery, the patient’s individual healing rate, the presence of any complications, and the specific recommendations of the surgeon or healthcare team.
- Short-term (days to weeks): Some procedures, like appendectomies or tonsillectomies, may require a soft food diet for only a few days or a couple of weeks.
- Medium-term (weeks to months): Surgeries involving the digestive system, such as gastric bypass or esophageal resections, often necessitate a soft food diet for several weeks to months to allow for adequate healing and adaptation.
- Long-term (months): In some cases, such as after extensive head and neck cancer surgery or in certain cases of esophageal stricture, a modified diet, including soft foods, may be required for a more extended period, possibly indefinitely.
General Guidelines for Soft Food Preparation
Following surgery, carefully preparing and consuming soft foods is crucial for a smooth recovery. This section provides guidance on safe and effective methods for preparing and handling soft foods, helping you navigate this phase with confidence. Adhering to these guidelines minimizes complications and promotes optimal healing.
Essential Cooking Methods for Soft Food Preparation
Several cooking methods are particularly well-suited for preparing soft foods. These techniques focus on breaking down food textures while retaining essential nutrients. Understanding and utilizing these methods will significantly enhance your ability to create appealing and easily digestible meals.
- Boiling and Simmering: Boiling involves cooking food in rapidly bubbling water, while simmering uses gently bubbling water. Both methods are ideal for softening vegetables, grains, and lean proteins. Simmering, in particular, helps to retain moisture and tenderness, preventing the food from drying out. For instance, consider simmering chicken breast until it’s easily shredded or boiling carrots until they’re fork-tender.
- Steaming: Steaming cooks food using steam, which preserves nutrients and flavors while maintaining a soft texture. This method is excellent for vegetables like broccoli, cauliflower, and green beans. A steamer basket placed over boiling water is a simple and effective way to steam foods.
- Baking: Baking can soften foods, especially when they are covered or cooked with added moisture. This method works well for casseroles, baked fish, and even some fruits. Ensure the food is cooked thoroughly to avoid any risk of undercooked portions.
- Pureeing: A food processor or blender is essential for creating smooth purees from various foods. This is especially helpful for fruits, vegetables, and cooked meats. Pureeing allows you to adjust the consistency to your tolerance level. Examples include pureeing cooked sweet potatoes or blending cooked chicken with broth.
- Mashing: Mashing involves breaking down food with a fork, potato masher, or other similar tools. This is suitable for softer foods like cooked potatoes, bananas, and avocados. Mashing retains some texture, making it a good option for those progressing beyond purees.
Foods to Avoid and Foods to Prioritize During the Soft Food Phase
Careful selection of foods is essential during the soft food phase. Prioritizing easily digestible, nutrient-rich options while avoiding foods that could cause discomfort or complications is crucial for a successful recovery.
- Foods to Avoid:
- Tough meats: Steak, pork chops, and other meats that are difficult to chew.
- Raw vegetables: Salads, raw carrots, and celery, which are hard to digest.
- Whole grains: Brown rice, quinoa, and other whole grains that may be too difficult to chew.
- Nuts and seeds: These can be difficult to digest and may cause irritation.
- Spicy foods: These can irritate the digestive system.
- Fried foods: These are often high in fat and can be difficult to digest.
- Carbonated beverages: These can cause bloating and discomfort.
- Foods to Prioritize:
- Cooked and pureed vegetables: Carrots, sweet potatoes, spinach, and other vegetables that are cooked until soft.
- Cooked and shredded lean proteins: Chicken, fish, and tofu, prepared in a soft and easily digestible form.
- Soft fruits: Bananas, cooked applesauce, and peaches, which are gentle on the digestive system.
- Dairy products: Yogurt and milk, which provide essential nutrients and are often well-tolerated.
- Cooked grains: White rice, oatmeal, and cream of wheat, which are easy to digest.
- Broth and soups: Broth-based soups with soft ingredients, providing hydration and nutrients.
Safe Food Handling Practices to Prevent Complications
Maintaining rigorous food safety practices is paramount during the soft food phase. Proper handling and storage of food minimize the risk of foodborne illnesses, which can significantly hinder recovery. Following these guidelines protects your health and supports the healing process.
- Wash Hands Thoroughly: Always wash your hands with soap and warm water for at least 20 seconds before preparing or eating food.
- Clean Surfaces and Utensils: Sanitize all countertops, cutting boards, and utensils before and after food preparation to prevent cross-contamination.
- Cook Food to Safe Temperatures: Use a food thermometer to ensure that all meats are cooked to their safe internal temperatures. For example, chicken should reach 165°F (74°C).
- Store Food Properly: Refrigerate perishable foods promptly, typically within two hours of preparation. Use airtight containers to prevent contamination and maintain freshness.
- Avoid Cross-Contamination: Prevent raw meat from coming into contact with cooked foods. Use separate cutting boards and utensils for raw and cooked items.
- Check Expiration Dates: Regularly check expiration dates on all food items and discard anything that is past its expiration date.
- Be Mindful of Leftovers: Consume leftovers within 3-4 days and reheat them thoroughly to an internal temperature of 165°F (74°C) to kill any bacteria.
Breakfast Ideas for Soft Food Diets
Following surgery, a well-balanced breakfast is crucial for kickstarting the healing process and providing essential nutrients. It’s important to choose meals that are easy to swallow and digest, minimizing discomfort and maximizing nutrient absorption. The following breakfast ideas are designed to be both nutritious and palatable, catering to the specific needs of individuals on a soft food diet.
Protein Intake Importance During Breakfast
Adequate protein intake is vital, particularly after surgery, for tissue repair and overall recovery. Protein helps rebuild damaged tissues, supports the immune system, and provides sustained energy throughout the morning. Aim to include a good source of protein in each breakfast meal to optimize healing and promote a feeling of fullness.
Breakfast Meal Ideas
Here are five breakfast ideas suitable for a soft food diet, presented in a table format:
| Meal | Ingredients | Preparation | Nutritional Benefits |
|---|---|---|---|
| Creamy Oatmeal with Soft Fruits | Cooked oatmeal (made with milk or a milk alternative), pureed soft fruits (banana, cooked applesauce, or peaches), a sprinkle of ground flaxseed. | Cook oatmeal according to package directions. Puree the fruit until smooth. Combine oatmeal and fruit, top with flaxseed. | Provides fiber, vitamins, and minerals from the fruit. Oatmeal offers complex carbohydrates for sustained energy. Flaxseed adds omega-3 fatty acids and fiber. |
| Scrambled Eggs with Cottage Cheese | 2-3 scrambled eggs (cooked until soft), 1/4 cup of cottage cheese (blended if needed), a pinch of salt and pepper. | Scramble eggs gently until cooked through but still soft. Blend cottage cheese if a smoother texture is desired. Combine eggs and cottage cheese. | Excellent source of protein for tissue repair. Cottage cheese provides calcium. Eggs offer choline for brain health. |
| Smoothie with Protein Powder | 1/2 cup of soft fruit (berries, banana), 1 scoop of protein powder (whey, soy, or pea protein), 1/2 cup of milk or milk alternative, a few ice cubes (optional). | Blend all ingredients until smooth. Adjust the consistency with more liquid as needed. | Protein powder supports muscle recovery and growth. Fruits contribute vitamins and antioxidants. Milk provides calcium and vitamin D. |
| Mashed Avocado with Soft Cooked Egg | 1/4 avocado (mashed), 1 soft-boiled egg (mashed), a pinch of salt and pepper. | Mash avocado until smooth. Mash the egg and combine with the avocado. Season to taste. | Avocado provides healthy fats and fiber. Eggs offer high-quality protein and essential nutrients. |
| Yogurt Parfait (Softened) | 1/2 cup of plain or vanilla yogurt (Greek yogurt is ideal), 1/4 cup of pureed fruit (mango or berries), a sprinkle of soft, cooked cereal (such as cream of wheat). | Layer yogurt, pureed fruit, and cereal in a small dish. Ensure the cereal is cooked until very soft. | Yogurt provides probiotics for gut health and protein. Fruits offer vitamins and antioxidants. Soft cereal adds carbohydrates for energy. |
Lunch and Dinner Recipes
Following surgery, adapting to a soft food diet can be challenging. However, with creativity and the right recipes, mealtimes can still be enjoyable and provide the necessary nutrients for recovery. The following recipes offer a variety of flavors and textures, ensuring a balanced intake of essential nutrients while remaining gentle on the digestive system.These recipes are designed to be easily modified to suit individual preferences and dietary restrictions.
Remember to always consult with a healthcare professional or registered dietitian for personalized dietary advice, especially after surgery.
Lunch and Dinner Recipe Ideas
To provide variety and ensure nutritional needs are met, a selection of five lunch and dinner recipes suitable for a soft food diet is presented below. These recipes emphasize ease of preparation and digestibility, utilizing common ingredients that can be adapted to individual taste preferences.
- Creamy Tomato Soup with Grilled Cheese Croutons: A classic comfort food, this soup provides essential vitamins and is easily consumed.
- Ingredients:
- 1 tbsp olive oil
- 1 onion, chopped
- 2 cloves garlic, minced
- 2 (28 ounce) cans crushed tomatoes
- 4 cups vegetable broth
- 1/2 cup heavy cream (or dairy-free alternative)
- Salt and pepper to taste
- For the croutons: 2 slices of bread, 1 slice of cheese (cheddar or similar), butter
- Preparation: Sauté onion and garlic in olive oil until softened. Add crushed tomatoes and vegetable broth. Simmer for 20 minutes. Blend until smooth. Stir in cream, season.
For croutons, butter bread and grill cheese between the slices. Cut into small cubes and serve with soup.
- Pureed Chicken and Vegetable Bowl: This recipe offers a protein-rich and balanced meal.
- Ingredients:
- 4 oz cooked chicken breast, chopped
- 1/2 cup cooked carrots, pureed
- 1/2 cup cooked peas, pureed
- 1/4 cup chicken broth
- Salt and pepper to taste
- Preparation: Puree chicken with carrots and peas until smooth. Add chicken broth to achieve desired consistency. Season with salt and pepper.
- Mashed Sweet Potato with Black Bean Puree: A flavorful and fiber-rich vegetarian option.
- Ingredients:
- 1 large sweet potato, peeled and cooked until soft
- 1/2 cup cooked black beans, pureed
- 1 tbsp olive oil
- Salt and cumin to taste
- Preparation: Mash sweet potato. Puree black beans with a little water to create a smooth consistency. Mix mashed sweet potato and black bean puree. Drizzle with olive oil and season.
- Scrambled Eggs with Avocado Mash: A quick and easy option packed with protein and healthy fats.
- Ingredients:
- 2 eggs
- 1 tbsp milk or cream
- Salt and pepper to taste
- 1/4 avocado, mashed
- Preparation: Scramble eggs with milk/cream and seasoning. Mash avocado separately. Serve eggs with avocado.
- Smooth Lentil Soup: A nutritious and easily digestible soup rich in fiber and protein.
- Ingredients:
- 1 tbsp olive oil
- 1 onion, chopped
- 1 carrot, chopped
- 1 celery stalk, chopped
- 1 cup red lentils, rinsed
- 4 cups vegetable broth
- Salt, pepper, and cumin to taste
- Preparation: Sauté onion, carrot, and celery in olive oil until softened. Add lentils and broth. Simmer until lentils are soft (about 20-25 minutes). Blend until smooth. Season.
Tips for Seasoning Soft Foods
Enhancing the flavor and palatability of soft foods is crucial for encouraging adequate nutrient intake during recovery. Proper seasoning can make meals more enjoyable and increase the likelihood of consuming sufficient calories and essential nutrients.
- Use Herbs and Spices: Fresh or dried herbs (such as parsley, dill, basil, and thyme) and spices (such as cumin, turmeric, and paprika) can add significant flavor without adding extra sodium or sugar.
- Add Acidic Elements: A squeeze of lemon or lime juice, a splash of apple cider vinegar, or a dollop of plain yogurt can brighten flavors and add complexity.
- Control Salt Intake: Be mindful of sodium levels, especially if you have any dietary restrictions. Use salt sparingly or explore low-sodium alternatives.
- Incorporate Flavorful Liquids: Broths, stocks, and vegetable juices can add depth of flavor to purees and soups.
- Consider Texture: Even with soft foods, different textures can add interest. For example, a small amount of finely grated cheese can add flavor and texture to a pureed vegetable dish.
Snack Ideas and Considerations
Snacking plays a vital role in maintaining energy levels and supporting healing during a soft food diet following surgery. Choosing the right snacks and managing portion sizes are crucial for preventing overeating and ensuring proper nutrient intake. This section details suitable snack options, emphasizing portion control and hydration strategies.
Suitable Snack Options
A variety of soft, easily digestible snacks can satisfy hunger and provide essential nutrients between meals. Prioritize options that are gentle on the digestive system and aligned with the overall dietary goals.
- Yogurt (Plain or Greek): Provides protein and calcium. Choose plain yogurt to control added sugar. Consider adding a small amount of pureed fruit for flavor.
- Smoothies: Blend fruits, vegetables, and protein sources like yogurt, protein powder, or silken tofu. Ensure all ingredients are soft and easily blended.
- Applesauce (Unsweetened): A good source of fiber and can help regulate digestion.
- Pudding (Sugar-Free or Low-Sugar): Choose pudding made with milk or a milk alternative for added nutrients.
- Mashed Avocado: Provides healthy fats and is easy to digest. Season with a pinch of salt.
- Soft Cooked Oatmeal: Prepare oatmeal with milk or water and ensure it’s cooked to a soft consistency. Add a small amount of pureed fruit or a drizzle of honey for flavor.
- Cottage Cheese: A good source of protein. Blend it for a smoother texture if needed.
- Banana: Naturally soft and easily digestible. Can be mashed or eaten as is.
- Well-Cooked, Pureed Vegetables: Options like carrots, sweet potatoes, or green beans, pureed until smooth.
Portion Sizes and Frequency of Snacking
Controlling portion sizes and snack frequency helps prevent overeating and supports steady energy levels.
- Portion Control: Serve snacks in small, measured portions. Aim for approximately 1/2 to 1 cup of a snack at a time, depending on the individual’s caloric needs and tolerance.
- Frequency: Plan for 2-3 snacks per day, ideally between meals, to prevent excessive hunger.
- Listen to Your Body: Pay attention to hunger and fullness cues. Stop eating when satisfied, not stuffed.
- Example: If a patient is prescribed a 1500-calorie diet, snacks should ideally range from 150 to 200 calories each.
Incorporating Hydration with Snacks
Adequate hydration is essential for recovery and overall well-being, particularly during a post-surgical soft food diet. Integrating fluids with snacks ensures sufficient fluid intake.
- Water: Always have water readily available. Drink a glass of water with each snack.
- Diluted Juice: Dilute fruit juice with water to reduce sugar intake while still providing flavor.
- Herbal Teas: Caffeine-free herbal teas can be soothing and provide hydration.
- Broth: Warm broth, such as chicken or vegetable broth, is a good source of electrolytes and fluids.
- Example: Pair a small serving of yogurt with a glass of water or a cup of herbal tea.
Beverages and Hydration Strategies
Maintaining adequate hydration is crucial during the recovery period following surgery, especially when consuming a soft food diet. Proper hydration aids in digestion, nutrient absorption, and overall healing. This section Artikels suitable beverage choices and strategies for staying adequately hydrated.
Suitable Beverage Choices
Selecting the right beverages can significantly impact your recovery. It is important to choose drinks that are easy to consume, gentle on the digestive system, and provide essential nutrients.
- Water: Water is the cornerstone of hydration and should be the primary beverage consumed. It supports all bodily functions and aids in the breakdown of food. Aim for consistent water intake throughout the day.
- Clear Broths: Broths, such as chicken or vegetable broth, are a good source of electrolytes and can be easily consumed. They can also add flavor and nutrients to the diet. Choose low-sodium options to avoid excessive salt intake.
- Diluted Juices: Diluted fruit juices, such as apple or grape juice, can provide some vitamins and hydration. Diluting them with water helps to reduce sugar concentration and potential digestive upset. Avoid citrus juices, which can be acidic.
- Herbal Teas: Caffeine-free herbal teas, like chamomile or peppermint, can be soothing and hydrating. Ensure the teas are lukewarm or cool, not hot, to avoid irritating the throat.
- Milk and Dairy Alternatives: Milk, or plant-based milk alternatives such as almond or soy milk, can provide protein and calcium. They should be consumed in moderation and tolerated well.
Strategies for Staying Adequately Hydrated
Developing a plan to ensure sufficient fluid intake is key. Several strategies can help maintain optimal hydration levels.
- Set Reminders: Set alarms or use apps to remind yourself to drink fluids regularly throughout the day. Aim to sip water consistently rather than consuming large quantities at once.
- Carry a Water Bottle: Keep a water bottle with you at all times to encourage frequent sips. Refill it throughout the day to monitor your intake.
- Track Your Intake: Keep a log of your fluid intake to monitor your progress and identify any patterns of dehydration. This can help you adjust your strategy as needed.
- Hydrate with Meals: Drink fluids with each meal, such as water or broth. This aids in digestion and helps you meet your daily fluid goals.
- Listen to Your Body: Pay attention to your body’s signals. Thirst is a key indicator of dehydration. Drink fluids whenever you feel thirsty.
Homemade Electrolyte Drinks
Electrolyte drinks help replace minerals lost through sweat, vomiting, or diarrhea. Making your own electrolyte drinks can be a cost-effective and healthy alternative to commercially available options.
A simple recipe for a homemade electrolyte drink:
- Ingredients:
- 4 cups of water
- 1/4 teaspoon of sea salt (provides sodium)
- 2 tablespoons of honey or maple syrup (for energy and potassium)
- 1/4 cup of lemon or lime juice (for flavor and potassium)
- Instructions: Combine all ingredients in a container and stir until the salt and honey/maple syrup are dissolved. Refrigerate and consume as needed.
Another example of an electrolyte drink using coconut water:
- Ingredients:
- 1 cup of coconut water (provides electrolytes, especially potassium)
- 1/4 cup of water
- Pinch of sea salt
- 1 tablespoon of lemon or lime juice
- Instructions: Mix all ingredients together and consume.
Consider these recipes as examples and adapt them to your personal preferences and needs. Always consult with your healthcare provider or a registered dietitian for personalized advice.
The World Health Organization (WHO) recommends oral rehydration solutions (ORS) for treating dehydration. Homemade electrolyte drinks can be a useful alternative, especially if commercial ORS is unavailable.
Food Textures and Consistency
Managing food textures and consistency is crucial for a successful recovery after surgery. The ability to swallow and digest food can be significantly impacted by surgical procedures, making it essential to adjust the texture of foods to match the patient’s current capabilities and stage of healing. Careful attention to texture not only aids in comfortable eating but also plays a vital role in preventing complications.
Comparing Food Textures for Recovery Stages
The progression of food textures often follows a phased approach, starting with the easiest to swallow and gradually increasing in complexity as the patient recovers. Understanding these textures is vital for safe and effective dietary management.
- Clear Liquids: This is typically the first stage after surgery. These foods are transparent and easily swallowed, leaving minimal residue. Examples include broth, clear juices (apple, cranberry), and gelatin. These are easily digestible and provide hydration.
- Important Consideration: Clear liquids offer minimal calories and nutrients, so they are intended for short-term use.
- Full Liquids: Full liquids include all clear liquids, plus opaque liquids and foods that are liquid at room temperature. Examples include milk, yogurt, blended soups (without chunks), and strained cream of wheat. This stage introduces more nutrients.
- Important Consideration: Patients should monitor their tolerance to dairy products at this stage.
- Pureed Foods: Pureed foods have a smooth, pudding-like consistency. Any food can be pureed, including cooked vegetables, fruits, meats, and grains. These foods are easily swallowed and require minimal chewing.
- Examples: Pureed applesauce, mashed sweet potatoes, and pureed chicken.
- Important Consideration: Texture should be uniform with no lumps or strings.
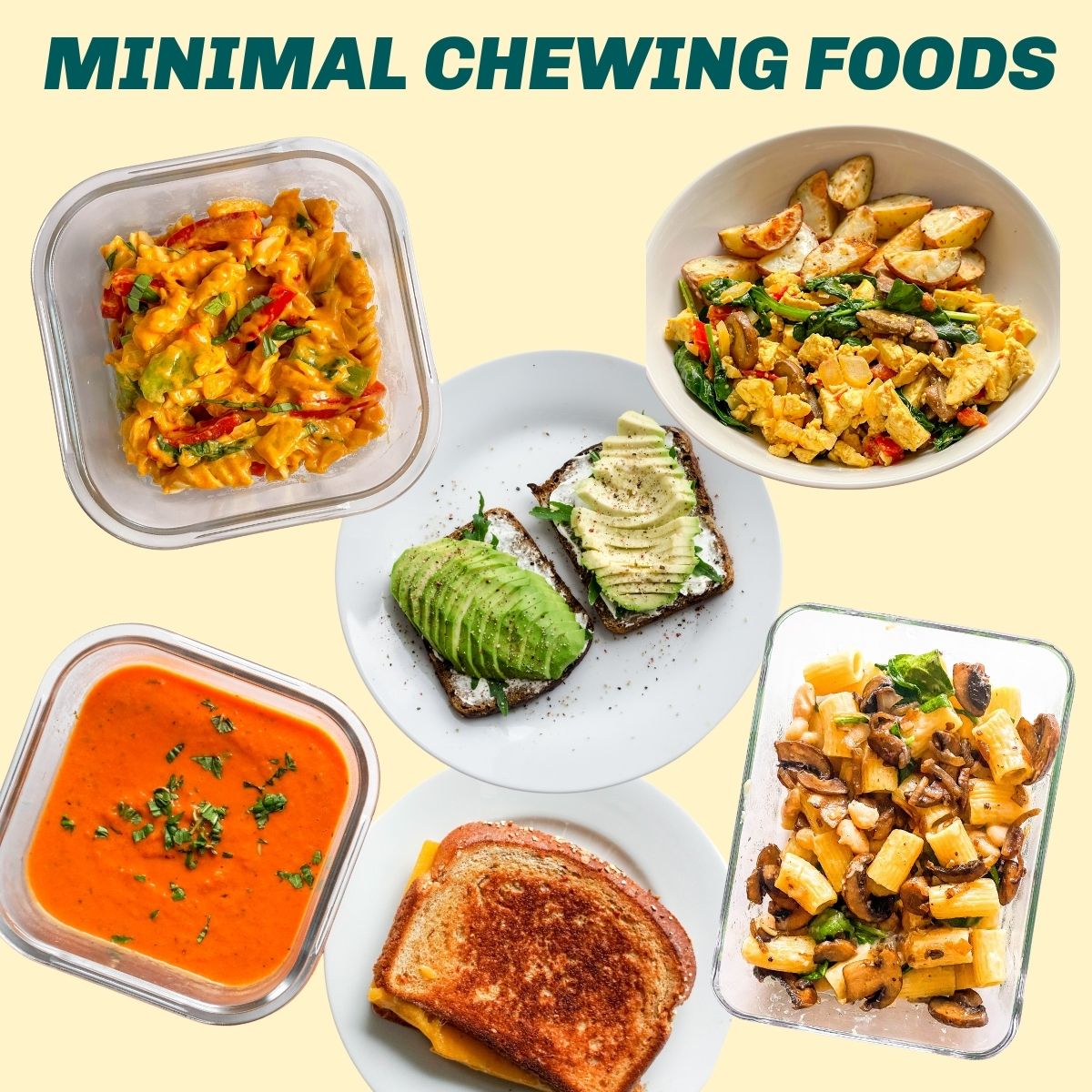
- Soft Foods: Soft foods are easily chewed and swallowed, with a slightly more defined texture than pureed foods. They should be tender and moist. Examples include scrambled eggs, well-cooked pasta, soft cooked vegetables, and ground meats with gravy.
- Examples: Mashed potatoes, cooked carrots, and tuna salad (without excessive mayonnaise).
- Important Consideration: Avoid foods that are difficult to chew or swallow, such as raw vegetables or tough meats.
- Regular Foods: Regular foods are introduced gradually as the patient tolerates them. This stage involves a return to the patient’s normal diet, with a focus on balanced nutrition.
- Important Consideration: Introduce new foods slowly and monitor for any adverse reactions.
Methods for Achieving Desired Food Consistency
Preparing food to the correct consistency involves several techniques and considerations to ensure safety and palatability. The goal is to make the food easy to swallow and digest without compromising its nutritional value.
- Blending and Pureeing: Blenders and food processors are essential tools for achieving a smooth consistency. Add liquid, such as broth, water, or juice, gradually to achieve the desired consistency.
- Example: To puree cooked chicken, add chicken broth slowly until the mixture is smooth.
- Mashing and Forking: Use a fork or potato masher to break down foods into a soft, easily manageable consistency. This method is suitable for foods like cooked vegetables and fruits.
- Example: Mashed potatoes can be made smoother by adding milk and butter.
- Thinning with Liquids: Add liquids such as broth, milk, or water to foods to thin them and make them easier to swallow. This is useful for soups, stews, and pureed foods.
- Example: Adding broth to oatmeal to achieve a thinner consistency.
- Cooking Techniques: Proper cooking methods can also affect food consistency. Cooking foods until they are tender and soft is crucial.
- Example: Steaming or boiling vegetables until they are soft enough to mash easily.
- Using Thickening Agents: For patients who have difficulty swallowing thin liquids, thickening agents such as commercial thickeners, cornstarch, or tapioca starch can be added.
- Important Consideration: Follow package instructions carefully to avoid over-thickening.
Importance of Food Texture in Preventing Complications
The texture of food plays a critical role in preventing complications, particularly aspiration. Aspiration occurs when food or liquid enters the lungs instead of the esophagus, leading to potential pneumonia or other respiratory infections.
- Preventing Aspiration: Choosing the right food texture reduces the risk of aspiration. Pureed and soft foods are less likely to cause aspiration than foods with large chunks or inconsistent textures.
- Example: A patient with swallowing difficulties should avoid dry, crumbly foods.
- Easing Swallowing: Foods that are easier to swallow reduce the effort required for eating, promoting better nutrition and hydration.
- Example: Offering smooth yogurt instead of a lumpy cottage cheese.
- Reducing Choking Hazards: Certain food textures pose a choking hazard. Avoiding these textures is crucial for safety.
- Foods to Avoid: Nuts, seeds, raw vegetables, and hard candies.
- Promoting Healing: Proper nutrition, supported by appropriate food textures, promotes wound healing and overall recovery.
- Example: Ensuring the patient consumes adequate protein through easily digestible sources like pureed meats.
- Enhancing Patient Compliance: Making food palatable and easy to eat increases patient compliance with dietary recommendations.
- Example: Offering well-seasoned, pureed foods that are visually appealing.
Nutritional Considerations and Supplements
Recovering from surgery demands increased nutritional needs to facilitate healing and restore strength. A well-balanced diet, even when restricted to soft foods, is crucial. This section Artikels the essential nutrients, supplementation considerations, and strategies to address potential deficiencies during the recovery phase.
Essential Nutrients Required During Recovery
The body’s demand for specific nutrients increases after surgery. These nutrients support tissue repair, immune function, and overall recovery. Prioritizing these nutrients in your soft food diet is paramount for optimal healing.
- Protein: Protein is the building block of tissues. It’s essential for wound healing and muscle recovery. Increased protein intake is necessary to counteract muscle loss often associated with inactivity and stress after surgery. Examples of high-protein soft food sources include pureed chicken, soft scrambled eggs, Greek yogurt, and protein shakes.
- Calories: Adequate caloric intake provides the energy needed for healing and maintaining body functions. Surgery can increase the body’s energy expenditure. Aim for calorie-dense soft foods like smoothies with added nut butter or avocados, to help meet your caloric needs without overfilling your stomach.
- Vitamin C: Vitamin C plays a crucial role in collagen synthesis, which is vital for wound healing. It also boosts the immune system. Good sources of vitamin C in a soft food diet include pureed fruits like cooked berries and soft citrus fruits (oranges, tangerines).
- Vitamin A: Vitamin A is involved in tissue repair and immune function. Pureed sweet potatoes, carrots, and spinach are excellent sources of Vitamin A that can be easily incorporated into a soft food diet.
- Zinc: Zinc is essential for wound healing and immune function. Incorporate zinc-rich soft foods such as pureed meats (chicken, turkey), and fortified cereals.
- Iron: Iron is necessary for red blood cell production and oxygen transport. Pureed meats, fortified cereals, and cooked spinach provide iron.
- Fluids: Maintaining adequate hydration is essential for all bodily functions, including nutrient transport and waste removal. Drink plenty of water, broth, and other hydrating beverages.
Incorporating Supplements to Support Healing
While a balanced soft food diet should be the primary source of nutrients, supplements may be necessary to support healing, especially if dietary intake is limited or specific nutrient deficiencies are identified. Consult your healthcare provider before starting any supplements.
- Protein Supplements: Protein shakes or powders can help meet increased protein needs, particularly when appetite is low. Whey protein, casein protein, and plant-based protein powders are available. Consider protein-enriched yogurts or puddings.
- Vitamin Supplements: A multivitamin can help ensure adequate intake of essential vitamins, including Vitamin C and Vitamin A. Your doctor may recommend a specific supplement based on your individual needs.
- Zinc Supplements: If zinc deficiency is suspected, a zinc supplement may be recommended. Follow your doctor’s instructions for dosage.
- Iron Supplements: If iron deficiency anemia is present, iron supplements may be necessary. Iron supplements can cause constipation; discuss this with your doctor.
- Probiotics: Surgery and antibiotic use can disrupt gut bacteria. Probiotics may help restore a healthy gut microbiome, aiding digestion and nutrient absorption.
Potential Nutrient Deficiencies and Mitigation Strategies
Certain nutrient deficiencies are more likely during recovery. Addressing these deficiencies promptly can improve healing outcomes.
- Protein Deficiency: Inadequate protein intake can lead to delayed wound healing, muscle loss, and weakened immune function. Ensure adequate protein intake through protein-rich soft foods and consider protein supplements if needed.
- Iron Deficiency Anemia: Post-surgical blood loss and poor dietary intake can contribute to iron deficiency anemia. Consume iron-rich foods and consider iron supplements if prescribed by your doctor.
- Vitamin Deficiencies: Limited food choices and reduced appetite can lead to vitamin deficiencies, particularly vitamins C and A. Focus on including vitamin-rich foods in your soft food diet. Consider a multivitamin.
- Fiber Deficiency: Constipation is a common problem after surgery, exacerbated by a soft food diet and pain medication. Increase fiber intake through soft, high-fiber foods like pureed fruits, cooked vegetables, and consider a fiber supplement if necessary.
- Strategies to Mitigate Deficiencies:
- Consult a Healthcare Professional: Work with your doctor or a registered dietitian to assess your nutritional needs and identify any deficiencies.
- Prioritize Nutrient-Dense Foods: Choose soft foods that are rich in essential nutrients, such as protein, vitamins, and minerals.
- Supplement Wisely: Use supplements as directed by your healthcare provider to address specific deficiencies.
- Monitor Your Symptoms: Be aware of any symptoms of nutrient deficiencies, such as fatigue, weakness, or poor wound healing, and report them to your doctor.
Managing Common Post-Surgery Dietary Challenges
Following surgery, your body requires specific care, and the dietary adjustments can sometimes lead to uncomfortable side effects. Understanding how to manage these challenges is crucial for a smoother recovery. This section focuses on addressing common post-surgical dietary issues and providing practical solutions to alleviate discomfort.
Managing Constipation on a Soft Food Diet
Constipation is a frequent complaint after surgery, often due to pain medication, decreased activity, and changes in diet. The soft food diet, while necessary, may lack the fiber needed for regular bowel movements. Addressing constipation requires a multifaceted approach.
- Increase Fluid Intake: Staying well-hydrated is paramount. Aim to drink at least eight glasses of water per day. Fluids help soften stools, making them easier to pass.
- Choose Fiber-Rich Soft Foods: Incorporate foods naturally higher in fiber, even if they are soft.
- Cooked vegetables like spinach, carrots, and sweet potatoes provide fiber.
- Well-cooked, soft fruits like pears and peaches can help.
- Consider Stool Softeners: Over-the-counter stool softeners, such as docusate sodium, can be helpful. Consult your doctor before taking any medication.
- Gentle Exercise: Light activity, such as walking, can stimulate bowel movements. Begin with short walks and gradually increase the duration and intensity as tolerated.
- Avoid Constipating Foods: Limit consumption of foods known to cause constipation, such as processed foods and excessive dairy products, if tolerated.
Addressing Nausea and Vomiting
Nausea and vomiting can significantly hinder recovery by making it difficult to consume adequate nutrients. Identifying and managing the causes is key.
- Eat Small, Frequent Meals: Instead of three large meals, try eating small portions every two to three hours. This can prevent overwhelming the digestive system.
- Avoid Strong Odors: Strong smells can trigger nausea. Ensure adequate ventilation in the kitchen and eating areas.
- Choose Bland Foods: Opt for bland, easily digestible foods.
- Examples include plain crackers, toast, and clear broths.
- Stay Hydrated: Sip clear liquids throughout the day to prevent dehydration, even if you cannot eat solid food.
- Examples of clear liquids include water, clear broth, and diluted juice.
- Ginger: Ginger has anti-nausea properties. Consider ginger ale (with real ginger), ginger tea, or ginger candies.
- Medications: Your doctor may prescribe anti-nausea medications. Take these as directed.
Coping with Loss of Appetite
Loss of appetite is a common side effect of surgery and medication. It’s crucial to find strategies to encourage eating, even when you don’t feel hungry.
- Eat at Scheduled Times: Even if you don’t feel hungry, try to eat at regular mealtimes. This can help regulate your body’s natural hunger cues.
- Make Food Appealing: Prepare meals that look and smell appetizing. Use garnishes and colorful plates to make food more inviting.
- Eat Nutrient-Dense Foods: Focus on consuming foods that are high in calories and nutrients.
- Examples include avocado, eggs, and full-fat yogurt.
- Boost Flavor: Use herbs, spices, and sauces to enhance the flavor of your food.
- Add a squeeze of lemon or a sprinkle of fresh herbs.
- Eat with Others: If possible, eat meals with family or friends. Social interaction can often stimulate appetite.
- Use Nutritional Supplements: If you struggle to consume enough calories, consider using nutritional supplements.
- Consult your doctor or a registered dietitian for recommendations.
Sample Meal Plan for a Day
Creating a structured meal plan is crucial when adhering to a soft food diet after surgery. This plan provides guidance on what to eat, when to eat, and the nutritional value of each meal. It helps ensure adequate nutrient intake while remaining within the dietary restrictions imposed by the surgery. Following a well-defined meal plan can aid in a smoother recovery process.
Daily Soft Food Meal Schedule
The following table presents a sample meal plan for a single day on a soft food diet. This plan includes meal times, portion sizes, and specific food choices. It is designed to provide a balanced intake of nutrients while remaining easy to consume and digest. This is a sample and individual needs may vary, so consulting with a healthcare professional or registered dietitian is always recommended.
| Time | Meal | Food | Nutritional Information (Approximate) |
|---|---|---|---|
| 8:00 AM | Breakfast | Cream of Wheat (1/2 cup) with mashed banana (1/2 medium) and a small amount of milk (1/4 cup). | Calories: 250, Protein: 8g, Carbohydrates: 45g, Fiber: 4g |
| 10:00 AM | Mid-Morning Snack | Plain yogurt (1/2 cup) blended with a small amount of soft cooked fruit (e.g., peaches, 1/4 cup). | Calories: 100, Protein: 7g, Carbohydrates: 15g, Fiber: 1g |
| 12:00 PM | Lunch | Pureed lentil soup (1 cup) with a small amount of cooked, pureed chicken (2 oz). | Calories: 300, Protein: 20g, Carbohydrates: 35g, Fiber: 8g |
| 2:00 PM | Afternoon Snack | Applesauce (1/2 cup) with a small amount of smooth peanut butter (1 tablespoon). | Calories: 150, Protein: 5g, Carbohydrates: 20g, Fiber: 2g |
| 6:00 PM | Dinner | Pureed salmon (3 oz) with mashed sweet potatoes (1/2 cup) and steamed, pureed green beans (1/2 cup). | Calories: 400, Protein: 25g, Carbohydrates: 40g, Fiber: 6g |
| 8:00 PM | Evening Snack | Custard or pudding (1/2 cup). | Calories: 150, Protein: 5g, Carbohydrates: 20g, Fiber: 0g |
Adapting Recipes for Different Dietary Needs
Adjusting recipes to accommodate individual dietary needs is crucial for ensuring nutritional adequacy and promoting recovery after surgery. Dietary restrictions can vary widely, encompassing conditions like diabetes, allergies, and intolerances. Understanding how to modify recipes safely and effectively allows patients to enjoy a wider variety of soft foods while adhering to their specific dietary requirements.
Modifying Recipes for Dietary Restrictions
Adapting recipes requires careful consideration of ingredients and their impact on specific health conditions. It is essential to replace or modify ingredients to align with the individual’s dietary needs.
- Diabetes Management: Individuals with diabetes need to carefully manage carbohydrate intake and glycemic index. Recipe adaptations may involve:
- Using low-glycemic index carbohydrates such as whole grains (e.g., quinoa, brown rice) instead of refined grains (e.g., white rice, pasta).
- Incorporating healthy fats like olive oil and avocado to slow carbohydrate absorption.
- Reducing added sugars and using sugar substitutes (in moderation) like stevia or erythritol.
- Monitoring portion sizes to control carbohydrate intake.
- Allergy Management: Food allergies require strict avoidance of allergenic ingredients. Common allergens include:
- Dairy: Replace dairy products with dairy-free alternatives like almond milk, soy milk, or coconut yogurt.
- Gluten: Use gluten-free flours (e.g., almond flour, rice flour) and gluten-free bread options.
- Nuts: Substitute nut butters with seed butters (e.g., sunflower seed butter, tahini).
- Soy: Avoid soy-based products and choose alternatives.
- Carefully read all food labels to identify and avoid allergens.
- Other Intolerances and Conditions: Adaptations may be necessary for conditions like lactose intolerance or celiac disease.
- Lactose Intolerance: Choose lactose-free dairy products or plant-based alternatives.
- Celiac Disease: Strictly avoid gluten-containing ingredients.
- FODMAP Intolerance: Limit high-FODMAP foods (e.g., onions, garlic, certain fruits) and use low-FODMAP alternatives.
Examples of Recipe Modifications
Here are specific examples of how to adapt recipes for various dietary needs.
- Chicken and Vegetable Soup (for Diabetes):
- Replace white rice with brown rice or quinoa.
- Add non-starchy vegetables (e.g., broccoli, spinach, zucchini) for fiber and nutrients.
- Use lean chicken breast and limit added salt.
- Smoothie (for Dairy Allergy):
- Use almond milk, soy milk, or coconut milk instead of cow’s milk.
- Include a protein source like soy protein powder or pea protein powder.
- Add fruits with lower sugar content, such as berries.
- Mashed Sweet Potatoes (for Gluten Sensitivity):
- Mashed sweet potatoes are naturally gluten-free.
- Season with olive oil, herbs, and spices.
- Ensure all added ingredients (e.g., seasonings, broth) are gluten-free.
Importance of Consulting with a Healthcare Professional
Personalized dietary advice is best obtained through consultation with healthcare professionals. A registered dietitian or a healthcare provider can assess an individual’s specific needs and create a tailored dietary plan.
- Individualized Assessment: A healthcare professional will evaluate the patient’s medical history, dietary restrictions, and nutritional needs.
- Personalized Recommendations: They can provide specific guidance on recipe modifications, portion sizes, and appropriate food choices.
- Supplement Recommendations: They may recommend supplements to address any nutritional deficiencies.
- Ongoing Support: Regular follow-up appointments can help monitor progress and adjust the diet as needed.
Food Safety and Hygiene
Following surgery, your immune system may be temporarily weakened, making you more susceptible to foodborne illnesses. Strict adherence to food safety and hygiene practices is crucial when preparing and consuming soft foods to minimize the risk of infection and ensure a smooth recovery. This section details essential practices to safeguard your health.
Essential Food Safety Practices
Implementing proper food safety practices is paramount when preparing soft foods, especially after surgery. This includes diligent handwashing, proper food handling, and thorough cooking techniques to eliminate harmful bacteria.
- Handwashing: Always wash your hands thoroughly with soap and warm water for at least 20 seconds before preparing food, after handling raw meat, poultry, or seafood, and after using the restroom.
- Clean Surfaces and Utensils: Sanitize all countertops, cutting boards, and utensils with hot, soapy water before and after food preparation. Use separate cutting boards for raw meats and other foods to prevent cross-contamination.
- Proper Cooking Temperatures: Cook all foods to the recommended internal temperatures to kill harmful bacteria. Use a food thermometer to ensure accuracy. For example:
- Poultry: 165°F (74°C)
- Ground meats: 160°F (71°C)
- Fish: 145°F (63°C)
- Preventing Cross-Contamination: Avoid cross-contamination by separating raw meats, poultry, and seafood from other foods. Store these items on the lowest shelves of your refrigerator to prevent drips onto other foods.
- Food Handling: Use separate utensils and cutting boards for raw and cooked foods. Wash all utensils and cutting boards thoroughly with hot, soapy water after each use.
- Thawing Food Safely: Thaw frozen foods in the refrigerator, in cold water (changing the water every 30 minutes), or in the microwave. Never thaw food at room temperature.
- Inspect Food Packaging: Check the expiration dates on all food items and discard any food that has passed its “use by” or “best by” date. Inspect packaging for any signs of damage, such as tears or leaks.
Safe Storage Practices
Proper food storage is vital to prevent bacterial growth and maintain the quality of your soft foods. This involves correct refrigeration, freezer storage, and pantry organization.
- Refrigeration: Store perishable soft foods in the refrigerator at 40°F (4°C) or below. This slows the growth of bacteria.
- Refrigerator Organization: Place cooked foods and ready-to-eat items on the top shelves of the refrigerator to prevent cross-contamination. Raw meats, poultry, and seafood should be stored on the bottom shelves.
- Freezer Storage: Freeze soft foods in airtight containers or freezer bags to prevent freezer burn and maintain quality. Label and date all frozen items.
- Pantry Storage: Store dry goods, such as canned goods and packaged foods, in a cool, dry place. Keep pantry items off the floor and away from direct sunlight.
- Proper Sealing: Always seal food containers tightly to prevent spoilage and contamination.
- Food Containers: Use food-grade containers for storing food. Avoid using containers that are not intended for food storage.
Handling Leftovers Safely
Proper handling of leftovers is essential to prevent foodborne illnesses. Following these guidelines ensures the safety of your meals after surgery.
- Cooling Leftovers: Cool leftovers quickly by dividing large portions into smaller, shallow containers. This allows for faster cooling and reduces the risk of bacterial growth.
- Refrigeration of Leftovers: Refrigerate leftovers within two hours of cooking. If the ambient temperature is above 90°F (32°C), refrigerate within one hour.
- Reheating Leftovers: Reheat leftovers thoroughly to an internal temperature of 165°F (74°C). Ensure food is steaming hot throughout.
- Discarding Leftovers: Discard leftovers after 3-4 days in the refrigerator. If you are unsure about the safety of a leftover, it is best to discard it.
- Smell and Appearance: If leftovers have an unusual odor, color, or texture, discard them immediately. Do not taste food to determine if it is safe.
- Avoid Tasting: Never taste food that looks or smells questionable. It’s always better to err on the side of caution.
Shopping List for Soft Food Ingredients
Planning your grocery shopping is crucial for a successful soft food diet after surgery. A well-organized shopping list ensures you have the necessary ingredients on hand to prepare nutritious and appealing meals. This reduces stress and helps you adhere to your dietary guidelines, supporting your recovery process.Here’s a sample shopping list, organized by food groups, to help you plan for a week of soft food meals.
This list provides a balanced variety of options, but feel free to adjust it based on your specific dietary needs and preferences. Remember to consult with your doctor or a registered dietitian for personalized recommendations.
Sample Shopping List
To make your shopping trip efficient and effective, here’s a sample shopping list broken down by food groups. This list covers a range of ingredients that can be adapted to create various soft food recipes.
- Protein Sources:
- Cooked, shredded chicken breast (pre-cooked or raw)
- Ground turkey or chicken (for making soft meatballs or patties)
- Eggs (for scrambled eggs and custards)
- Plain Greek yogurt (high in protein and probiotics)
- Canned tuna or salmon (packed in water, drained)
- Tofu (silken or soft, for blending)
- Lentils (cooked, for pureeing)
- Dairy and Alternatives:
- Milk (cow’s milk, almond milk, soy milk, or other alternatives)
- Plain yogurt (Greek or regular)
- Cottage cheese (smooth texture)
- Cheese (soft cheeses like ricotta or cream cheese)
- Fruits:
- Bananas (ripe, for easy mashing)
- Avocados (ripe, for mashing)
- Applesauce (unsweetened)
- Peaches or pears (canned in juice, drained and mashed)
- Berries (fresh or frozen, for blending into smoothies)
- Vegetables:
- Sweet potatoes (for mashing)
- Carrots (cooked and pureed)
- Spinach (cooked and pureed)
- Broccoli florets (cooked and pureed)
- Green beans (cooked and pureed)
- Canned pumpkin puree
- Grains and Starches:
- Oatmeal (rolled oats, for cooking into a soft consistency)
- White rice (cooked, for blending or eating soft)
- Pasta (cooked very soft)
- Bread (for toast or bread pudding, if tolerated)
- Fats and Oils:
- Olive oil (for cooking and adding flavor)
- Avocado oil (for cooking)
- Butter (small amounts, for flavor)
- Condiments and Seasonings:
- Salt
- Pepper
- Herbs (fresh or dried, such as basil, oregano, thyme)
- Spices (such as cinnamon, nutmeg)
- Broth (chicken, vegetable, or bone broth)
- Honey or maple syrup (for a touch of sweetness)
Tips for Efficient Grocery Shopping
To make your grocery shopping experience as smooth as possible, consider these tips:
- Plan Ahead: Review your meal plan and make a detailed shopping list.
- Check Your Pantry: Before you go shopping, check your pantry and refrigerator to avoid buying items you already have.
- Shop Strategically: Organize your list by grocery store sections (produce, dairy, meat, etc.) to save time.
- Read Labels: Pay attention to nutrition labels, especially sodium and sugar content. Choose low-sodium and low-sugar options whenever possible.
- Consider Pre-Prepared Options: If you are limited on time or energy, consider buying pre-cooked chicken, pre-cut vegetables, or other convenience items. However, always read labels carefully.
- Don’t Shop Hungry: Shopping while hungry can lead to impulse purchases and unhealthy choices.
- Ask for Help: Don’t hesitate to ask store employees for help locating items.
- Store Properly: Upon returning home, properly store your groceries to maintain freshness and prevent spoilage. Follow the recommended storage guidelines for each food item.
Emotional and Psychological Aspects of Dietary Changes
Adjusting to a soft food diet after surgery often involves significant emotional and psychological adjustments alongside the physical changes. The restrictions on food choices and textures can impact a person’s mood, self-perception, and social interactions. Understanding and addressing these emotional aspects is crucial for a smoother recovery and overall well-being.
Emotional Impact of Dietary Changes
The emotional impact of a soft food diet can manifest in various ways, ranging from mild frustration to more significant emotional distress. This is because food is often associated with comfort, celebration, and social connection.
- Frustration and Irritability: The limitations on food choices can lead to feelings of frustration, especially if a person is accustomed to a wide variety of foods and textures. This can be exacerbated by the physical discomfort associated with surgery.
- Sadness and Loss: Individuals may experience sadness or a sense of loss related to the inability to enjoy favorite foods or participate in social events centered around eating. For example, missing out on a holiday meal or a dinner out with friends can trigger feelings of isolation.
- Anxiety and Worry: Concerns about adequate nutrition, potential complications from eating the wrong foods, or the long-term impact of dietary changes can cause anxiety. This is particularly true for individuals with pre-existing anxiety disorders.
- Body Image Concerns: Changes in diet, and the resulting weight fluctuations, can affect body image and self-esteem. This can be more pronounced if the surgery impacts the digestive system, leading to changes in bowel habits or bloating.
- Social Isolation: Dietary restrictions can make it challenging to participate in social gatherings and celebrations involving food. This can lead to feelings of isolation and loneliness.
Coping Strategies for Dealing with Food Restrictions
Effectively managing the emotional challenges of a soft food diet requires proactive coping strategies. These strategies aim to address negative emotions and promote a positive mindset.
- Focus on the Benefits: Remind yourself of the positive aspects of the diet, such as aiding healing, reducing discomfort, and preventing complications. Keep in mind the long-term health benefits.
- Set Realistic Expectations: Understand that the soft food diet is temporary and a necessary part of the recovery process. Avoid setting unrealistic expectations about how quickly you will adjust.
- Plan and Prepare Meals: Planning meals in advance and preparing soft food options can help manage cravings and reduce the feeling of deprivation. Experimenting with new recipes can also be enjoyable.
- Practice Mindful Eating: Pay attention to the taste, texture, and smell of the food. Eating slowly and savoring each bite can enhance the dining experience.
- Seek Professional Support: Consider talking to a therapist or counselor specializing in eating disorders or post-surgical recovery. They can provide coping strategies and emotional support.
- Engage in Other Enjoyable Activities: Find alternative activities that provide pleasure and distraction from food-related anxieties. This could include hobbies, exercise, or spending time with loved ones.
- Keep a Food Journal: Tracking your meals and how you feel can help identify triggers for emotional eating and patterns of negative emotions.
- Join a Support Group: Connecting with others who are going through similar experiences can provide a sense of community and shared understanding. Online and in-person support groups can offer valuable insights and encouragement.
Role of Support Systems in Recovery
A strong support system is essential for navigating the emotional and psychological challenges of a soft food diet. Support can come from various sources, including family, friends, healthcare professionals, and support groups.
- Family and Friends: Encourage family and friends to be understanding and supportive. Ask them to help with meal preparation, provide companionship, and avoid pressuring you to eat foods that are not allowed.
For example, a friend can bring over a pre-made soft food meal, offering both practical help and emotional support.
- Healthcare Professionals: Your doctor, dietitian, and other healthcare providers can offer valuable guidance and support. They can provide nutritional advice, address any concerns about your diet, and help manage any physical symptoms that are impacting your emotional state.
For instance, a dietitian can tailor a meal plan to your specific needs, while a doctor can monitor your progress and address any complications.
- Support Groups: Joining a support group, either online or in person, can provide a safe space to share experiences, receive encouragement, and learn from others. Support groups can offer a sense of community and reduce feelings of isolation.
Consider a support group where individuals share their experiences with post-surgical diets.
- Communication: Openly communicate your needs and feelings to your support system. Let them know how they can best support you during your recovery.
For example, you can inform your family that you’d prefer to eat a soft food meal together rather than them eating something you cannot.
- Setting Boundaries: It’s important to set boundaries with others to protect your emotional well-being. This might involve politely declining invitations to social events where food is a central focus, or asking for understanding when you are unable to eat certain foods.
For example, if someone offers you a food item that is not allowed, politely decline and explain your dietary restrictions.
Potential Complications and When to Seek Medical Advice
Adhering to a soft food diet post-surgery is crucial for recovery, but it’s essential to be aware of potential complications. Recognizing these issues early and knowing when to seek medical attention can significantly impact your healing process. This section Artikels possible complications, warning signs, and when to contact your healthcare provider.
Difficulty Swallowing or Painful Swallowing
Difficulty or pain while swallowing (dysphagia or odynophagia) can occur due to inflammation, swelling, or nerve damage related to the surgery. These symptoms may require prompt evaluation.
Nausea and Vomiting
Nausea and vomiting are common after surgery and can be exacerbated by certain foods or the inability to tolerate them. Persistent vomiting can lead to dehydration and electrolyte imbalances, necessitating medical intervention.
Constipation
A soft food diet, especially if not properly balanced with fiber-rich options, can contribute to constipation. Certain medications, reduced physical activity, and changes in diet can also be contributing factors. Addressing this promptly is crucial to prevent discomfort and potential complications.
Diarrhea
Conversely, some individuals may experience diarrhea, particularly if the digestive system is sensitive or if the diet includes foods that irritate the gut. Diarrhea can also lead to dehydration and electrolyte imbalances.
Inadequate Nutritional Intake
If the soft food diet is not carefully planned, there’s a risk of inadequate intake of essential nutrients, leading to delayed healing, muscle loss, and other nutritional deficiencies. Consulting a dietitian is recommended to ensure a balanced diet.
Wound Healing Problems
Poor nutrition can negatively impact wound healing. A deficiency in protein, vitamins, and minerals can slow down the healing process and increase the risk of infection.
Warning Signs Requiring Medical Attention
It’s crucial to recognize warning signs that indicate a need for medical intervention. These signs can range from mild discomfort to serious complications.
- Severe Abdominal Pain: Persistent or worsening abdominal pain, especially if accompanied by fever or other symptoms, may indicate a serious issue such as an infection, bowel obstruction, or internal bleeding.
- High Fever: A fever above 100.4°F (38°C) could signify an infection.
- Persistent Nausea and Vomiting: Inability to keep down fluids or food for more than a few hours can lead to dehydration and electrolyte imbalances.
- Significant Weight Loss: Losing a significant amount of weight rapidly can indicate inadequate caloric intake or malabsorption.
- Changes in Bowel Movements: Persistent diarrhea or constipation, especially if accompanied by blood in the stool, should be reported.
- Signs of Dehydration: These include decreased urination, dark urine, dizziness, and extreme thirst.
- Chest Pain or Difficulty Breathing: These symptoms can indicate serious cardiovascular or respiratory issues.
- Increased Swelling, Redness, or Drainage at the Surgical Site: These signs may indicate an infection or other complications.
When to Contact Your Healthcare Provider
Contacting your healthcare provider promptly is essential when experiencing any of the warning signs. Early intervention can prevent minor issues from escalating into serious complications.
- Immediately: If you experience severe abdominal pain, high fever, chest pain, or difficulty breathing, seek immediate medical attention.
- Within 24 Hours: If you experience persistent nausea and vomiting, significant weight loss, or signs of dehydration, contact your healthcare provider within 24 hours.
- As Soon As Possible: For changes in bowel movements, increased swelling, redness, or drainage at the surgical site, contact your healthcare provider as soon as possible.
- Routine Check-Ups: Attend all scheduled follow-up appointments to monitor your progress and address any concerns.
Long-Term Dietary Considerations
The transition from a soft food diet after surgery back to a regular diet is a crucial step in the recovery process. This phase requires careful planning and adherence to guidelines to ensure optimal healing and long-term well-being. It is important to gradually reintroduce solid foods and maintain a balanced diet for sustained health benefits.
Browse the implementation of best food odessa tx in real-world situations to understand its applications.
Transitioning Back to a Regular Diet
The return to a regular diet is a progressive process, and the pace should be guided by individual tolerance and the surgeon’s recommendations. Rushing this process can lead to discomfort, digestive issues, and potentially hinder recovery.
Guidelines for Gradually Reintroducing Solid Foods
Reintroducing solid foods should be a structured process, paying close attention to how your body responds. This structured approach helps to minimize discomfort and allows for the digestive system to adapt gradually.
- Start with Easily Digestible Foods: Begin with foods that are gentle on the digestive system, such as cooked vegetables (e.g., carrots, green beans), soft fruits (e.g., bananas, cooked applesauce), and well-cooked grains (e.g., white rice, oatmeal).
- Introduce One New Food at a Time: Introduce new foods one at a time, allowing several days between introductions. This helps identify any foods that may cause discomfort or digestive upset.
- Chew Food Thoroughly: Emphasize the importance of chewing food thoroughly to aid digestion and reduce the burden on the digestive system. This is particularly important after surgery when the digestive system may be more sensitive.
- Monitor for Symptoms: Pay close attention to any symptoms such as bloating, gas, abdominal pain, nausea, or changes in bowel movements. If any symptoms arise, reduce the portion size or eliminate the newly introduced food until symptoms subside.
- Gradually Increase Fiber Intake: Fiber is essential for digestive health, but it should be introduced gradually. Start with small amounts of fiber-rich foods like whole grains and vegetables and increase as tolerated. Excessive fiber too soon can cause gas and bloating.
- Stay Hydrated: Adequate hydration is crucial for overall health and helps with the digestion of food. Drink plenty of water throughout the day.
- Avoid Processed Foods and Sugary Drinks: These can cause inflammation and digestive upset. Focus on whole, unprocessed foods.
Maintaining a Balanced Diet for Long-Term Health
Maintaining a balanced diet is critical for long-term health and well-being, especially after surgery. A balanced diet provides the necessary nutrients to support recovery, maintain energy levels, and prevent chronic diseases.
- Focus on Nutrient-Dense Foods: Prioritize foods that are rich in nutrients, such as fruits, vegetables, lean proteins, and whole grains. These foods provide essential vitamins, minerals, and antioxidants that support overall health.
- Include Adequate Protein: Protein is essential for tissue repair and muscle maintenance. Aim to include a good source of protein with each meal. Examples include lean meats, poultry, fish, beans, lentils, and tofu.
- Choose Healthy Fats: Healthy fats are important for brain function and overall health. Include sources of healthy fats such as avocados, nuts, seeds, and olive oil in your diet.
- Limit Processed Foods, Sugary Drinks, and Excessive Sodium: These foods can contribute to inflammation, weight gain, and other health problems. Focus on whole, unprocessed foods instead.
- Control Portion Sizes: Eating appropriate portion sizes is important for weight management and overall health. Be mindful of how much you are eating and avoid overeating.
- Stay Hydrated: Drink plenty of water throughout the day to support digestion, nutrient absorption, and overall health.
- Consider Supplements (if needed): In some cases, supplements may be necessary to address specific nutrient deficiencies. Consult with a healthcare professional to determine if supplements are appropriate for you. For example, after certain bariatric surgeries, patients may need to take lifelong supplements of vitamins like B12, D, and calcium to avoid deficiencies.
- Regular Physical Activity: Combine a healthy diet with regular physical activity to improve overall health and maintain a healthy weight. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, along with muscle-strengthening activities at least two days a week.
Using Kitchen Tools to Prepare Soft Foods
Preparing soft foods after surgery often necessitates the use of various kitchen tools to achieve the appropriate textures and consistencies for easy consumption and digestion. Understanding how to utilize these tools effectively can significantly enhance the dietary experience and facilitate a smoother recovery.
Essential Kitchen Tools
Several kitchen tools are particularly useful for preparing soft foods. These tools help break down food into manageable pieces, create purees, and achieve the desired smooth textures.
- Blender: A blender is essential for creating smooth purees from fruits, vegetables, and cooked meats. High-powered blenders can efficiently process tougher ingredients.
- Food Processor: A food processor is versatile and can chop, mince, puree, and blend various ingredients. It’s suitable for preparing larger quantities of food.
- Immersion Blender (Stick Blender): An immersion blender offers convenience, allowing you to blend directly in pots and bowls, reducing the need for extra dishes.
- Potato Masher: A potato masher is useful for mashing cooked potatoes, sweet potatoes, and other soft vegetables to a desired consistency.
- Sieve or Strainer: A sieve or strainer can remove any remaining lumps or seeds from purees, ensuring a completely smooth texture.
- Measuring Cups and Spoons: Accurate measurements are crucial for consistent results, especially when following recipes.
- Small Saucepan or Pot: Necessary for cooking vegetables, meats, and preparing sauces.
- Mixing Bowls: Useful for combining ingredients before processing or cooking.
- Rubber Spatula: Helpful for scraping down the sides of blenders and food processors to ensure all ingredients are processed evenly.
Using Blenders, Food Processors, and Other Tools
The techniques for using these tools are relatively straightforward, but understanding the nuances can improve the final product.
- Blender:
- Add liquids first to facilitate blending. This helps prevent the blender from jamming.
- Start on a low speed and gradually increase it to prevent splattering.
- Blend until the desired consistency is achieved. For purees, aim for a smooth, lump-free texture.
- If the mixture is too thick, add more liquid (broth, water, or milk) gradually.
- Food Processor:
- Use the chopping blade for chopping vegetables or meats.
- Use the shredding or slicing discs for preparing ingredients like shredded cheese or sliced fruits.
- Pulse the food processor for short bursts to control the texture, especially when pureeing.
- Avoid over-processing, which can result in a gummy texture.
- Immersion Blender:
- Submerge the blender head in the food and start blending.
- Move the blender around to ensure all ingredients are processed evenly.
- Be careful not to splatter the food, especially when using it in a hot pot.
- Potato Masher:
- Mash cooked potatoes or other vegetables directly in the pot.
- Add liquids (milk, broth, or butter) to improve the texture and flavor.
- Mash until the desired consistency is reached. Avoid over-mashing, which can make the food gluey.
- Sieve or Strainer:
- Place the puree in the sieve or strainer over a bowl.
- Use a spoon or spatula to push the puree through the mesh, removing any lumps or seeds.
- Discard any solids remaining in the sieve.
Benefits of Utilizing Kitchen Tools
Employing these kitchen tools provides several advantages during the recovery process.
- Improved Texture: Tools like blenders and food processors allow for creating smooth textures that are easy to swallow and digest, which is critical after surgery.
- Enhanced Nutrient Absorption: Pureeing or finely chopping food can make it easier for the body to absorb nutrients, which supports healing and recovery.
- Increased Food Variety: These tools enable the preparation of a wide range of soft food options, preventing dietary monotony and ensuring adequate nutrient intake.
- Reduced Chewing Effort: Soft foods prepared with these tools require minimal chewing, reducing strain on the jaw and promoting comfort.
- Customization: Kitchen tools allow for adapting food textures to meet individual needs and preferences, contributing to a more enjoyable eating experience.
Creative Ways to Present Soft Foods
Adjusting to a soft food diet after surgery can be challenging, and the appearance of meals can significantly impact a patient’s appetite and overall well-being. Presenting soft foods in an appealing manner can make the dietary transition more manageable and encourage better nutrition. This section explores techniques for enhancing the visual appeal of soft food meals, thereby promoting patient satisfaction and adherence to the dietary plan.
Enhancing Visual Appeal Through Plating Techniques
Creating visually appealing soft food dishes is crucial for stimulating appetite and encouraging consumption. Careful attention to color, texture, and arrangement can transform a simple meal into a more enjoyable experience.
- Color Coordination: Utilize a variety of colors to make the plate more attractive. This can involve using naturally colorful ingredients.
For example, a plate of pureed chicken might be garnished with a swirl of pureed carrots (orange), a small dollop of pureed spinach (green), and a sprinkle of finely chopped parsley (another green). - Texture Contrast: While all foods are soft, incorporating elements that mimic different textures can add interest.
For instance, a smooth puree of salmon could be topped with a sprinkle of finely crumbled cooked quinoa (which is also soft but has a slightly granular texture) or a few tiny pieces of avocado. - Arrangement and Portion Control: Avoid simply piling food on the plate.
Instead, use a clean plate and arrange the food in a visually appealing manner. Portion control is important, and arranging food in smaller, defined portions can make the meal seem less overwhelming. Use small ramekins or bowls for individual components. - Garnish and Presentation: Garnishes can significantly enhance the appeal of soft foods.
A simple sprig of fresh herbs (like mint or basil) or a swirl of flavored oil can elevate the presentation. Ensure garnishes are edible and safe for the patient to consume. - Use of Servingware: The choice of servingware can also impact the visual appeal.
Use plates, bowls, and utensils that are visually pleasing. Consider using smaller plates to make portions look more substantial.
Making Soft Food Meals More Appetizing
Beyond plating techniques, the overall composition and preparation of soft food meals can be adjusted to increase their appeal.
- Flavor Enhancement: Taste is paramount.
Soft foods can sometimes lack flavor, so it’s important to enhance them. Use herbs, spices, and flavorful broths or sauces to add depth of flavor. Avoid excessive salt, but experiment with other seasonings like garlic powder, onion powder, or paprika. - Temperature Considerations: Serve food at the appropriate temperature.
Hot foods should be served hot, and cold foods should be served cold. The temperature can significantly affect the taste and texture of the food. - Variety and Choice: Offer a variety of options to cater to individual preferences.
This can involve offering different pureed proteins, vegetables, and fruits. Rotate the menu regularly to prevent boredom. - Incorporating Familiar Foods: Include familiar foods that the patient enjoys.
This can make the transition to a soft food diet easier. For example, a patient who loves mashed potatoes might be happy to have a pureed version. - Adding Textural Variety (where appropriate): While the diet is soft, incorporating small amounts of slightly more textured elements (if tolerated) can be beneficial.
For instance, adding a few soft, cooked vegetables to a puree can provide a different mouthfeel. Always consult with a healthcare professional to ensure this is safe.
Making Meals Look More Appealing to Patients
Consideration of the patient’s perspective and preferences is essential for making soft food meals more appealing.
- Personalization: Whenever possible, personalize meals to the patient’s likes and dislikes.
Ask about their favorite foods and try to incorporate them into the diet, modified as necessary. - Involving the Patient: If appropriate, involve the patient in the meal planning process.
This can give them a sense of control and increase their willingness to eat the food. - Providing Information: Educate the patient about the nutritional benefits of the meals.
This can help them understand the importance of the diet and encourage them to eat it. - Creating a Positive Environment: Serve meals in a clean and comfortable environment.
A pleasant atmosphere can significantly improve the dining experience. - Using Creative Names: Give meals appealing names.
Instead of simply calling it “pureed chicken,” consider calling it “Creamy Herb-Infused Chicken Delight.” This can make the meal sound more exciting.
Addressing Taste Fatigue
The soft food phase following surgery can sometimes lead to a phenomenon known as taste fatigue. This occurs when the palate becomes desensitized or bored with the limited range of textures and flavors typically consumed during this period. Addressing taste fatigue is crucial for maintaining appetite, ensuring adequate nutrient intake, and promoting a positive recovery experience.
Incorporating Diverse Flavors
Variety is key to combating taste fatigue. The soft food diet doesn’t have to be bland. Strategic use of herbs, spices, and other flavorings can significantly enhance the taste and appeal of meals.
- Herbs: Fresh or dried herbs can add depth and complexity to dishes. Experiment with basil, oregano, thyme, rosemary, parsley, and cilantro. For example, pureed chicken can be elevated with fresh thyme and a touch of lemon zest.
- Spices: Spices provide a wide spectrum of flavors, from warm and earthy to spicy and vibrant. Consider using cumin, coriander, turmeric, ginger, cinnamon, nutmeg, and paprika. A mashed sweet potato can be enhanced with cinnamon and a pinch of nutmeg.
- Flavor Infusions: Infusing oils or broths with herbs and spices before adding them to soft foods can impart a more concentrated flavor. For instance, infuse olive oil with garlic and rosemary for a few hours before drizzling it over pureed vegetables.
- Citrus and Vinegar: A squeeze of fresh lemon or lime juice can brighten up a dish and cut through richness. A splash of balsamic or apple cider vinegar can add a tangy note. A simple pureed lentil soup can be significantly enhanced with a squeeze of lemon.
- Flavor Extracts: Use small amounts of extracts like vanilla or almond to add sweetness and aroma to purees and smoothies. Be mindful of sugar content.
- Salt and Pepper: While taste preferences vary, appropriate use of salt and pepper is important for enhancing flavors. Always follow your doctor’s recommendations regarding sodium intake.
Strategies for Meal Variety, Soft food ideas after surgery
Maintaining interest in meals is paramount to prevent boredom and ensure adherence to the soft food diet. Planning and mindful preparation can help keep meals exciting.
- Recipe Variations: Modify existing recipes by swapping ingredients or adding new flavor combinations. For example, a basic chicken puree can be transformed into a different meal by adding different vegetables, herbs, or spices.
- Global Cuisine Inspiration: Explore different cuisines for inspiration. Pureed versions of dishes from various cultures can offer diverse flavor profiles. For instance, a pureed version of Thai green curry or a mild Indian korma can introduce new tastes.
- Presentation Matters: Even soft foods can be presented in an appealing manner. Use different bowls and plates, and garnish with a sprinkle of herbs or a drizzle of flavored oil. A visually appealing meal can significantly enhance the dining experience.
- Texture Variations (Within Limits): While the diet focuses on soft foods, slight variations in texture can be introduced as tolerated. For example, adding small amounts of cooked and finely chopped vegetables to a puree can provide a subtle textural contrast. Always consult with your doctor or a registered dietitian before introducing new textures.
- Meal Rotation: Rotate meals to prevent monotony. Plan a weekly menu and alternate between different recipes and flavor profiles. Avoid eating the same meals repeatedly.
- Focus on Aromatics: The sense of smell greatly influences taste. Adding fragrant ingredients like garlic, onions, or ginger during cooking can enhance the overall flavor experience.
Conclusive Thoughts: Soft Food Ideas After Surgery
In conclusion, mastering soft food ideas after surgery is key to a successful post-operative journey. By understanding the principles of soft food preparation, meal planning, and potential challenges, you can significantly enhance your recovery. This guide provides the knowledge and tools necessary to navigate this dietary phase with confidence, ensuring optimal healing and a return to a balanced, healthy life. Remember to consult your healthcare provider for personalized dietary advice.


