Low oxalate foods for dogs are crucial for canine health, particularly for those prone to oxalate-related issues. This comprehensive guide will navigate the complexities of oxalates in your dog’s diet, providing you with the knowledge to make informed decisions about their nutrition. Understanding the impact of oxalates, identifying high-risk foods, and selecting suitable alternatives are all key components of this discussion.
We will delve into the potential health risks associated with high oxalate intake, such as the formation of calcium oxalate crystals, and explore practical strategies for managing oxalate levels. This includes examining food labels, understanding commercial food options, and even preparing homemade, low-oxalate meals for your furry friend. We’ll also explore the role of supplements and the importance of veterinary consultation.
Understanding Oxalates in Canine Diets
Oxalates are naturally occurring compounds found in various plants and, to a lesser extent, in animal tissues. While not inherently toxic in small amounts, excessive oxalate intake can pose significant health risks for dogs. Understanding the role of oxalates in canine nutrition is crucial for preventing certain health issues.
What Oxalates Are
Oxalates, also known as oxalic acid, are organic acids that bind with minerals, particularly calcium, in the body. This binding process can lead to the formation of insoluble crystals. These crystals are the primary concern regarding oxalate intake in dogs.
Potential Health Risks Associated with High Oxalate Intake
High oxalate intake can lead to several health problems in dogs. These risks primarily involve the urinary system, but can have broader implications.
- Kidney Stones: The most significant risk is the formation of calcium oxalate crystals in the kidneys and urinary tract. These crystals can aggregate and form stones, causing pain, urinary obstruction, and potentially kidney damage. The size and location of these stones can vary, with smaller stones potentially passing with urine and larger stones requiring surgical intervention.
- Kidney Damage: Prolonged exposure to high oxalate levels can damage the kidney tubules, leading to chronic kidney disease. This damage impairs the kidneys’ ability to filter waste products from the blood.
- Other Health Complications: Although less common, excessive oxalate intake may contribute to other health issues, including gastrointestinal problems and, in severe cases, systemic toxicity.
The Role of Oxalates in the Formation of Calcium Oxalate Crystals
The formation of calcium oxalate crystals is a complex process influenced by several factors, including dietary oxalate levels, calcium intake, urine pH, and the dog’s overall hydration status.
Here’s a breakdown of the process:
- Ingestion and Absorption: Dogs ingest oxalates through their diet. These oxalates are absorbed in the digestive tract and enter the bloodstream.
- Binding with Calcium: In the bloodstream and, more importantly, in the kidneys, oxalates bind with calcium.
- Crystal Formation: The calcium oxalate complex, when reaching a certain concentration, forms crystals.
- Crystal Aggregation: These microscopic crystals can then aggregate, forming larger stones.
- Factors Influencing Crystal Formation: The urine pH, the concentration of calcium and oxalates, and the presence of other substances in the urine can all affect crystal formation. A urine pH that is too acidic or too alkaline can promote crystal formation.
The formula for calcium oxalate is:
CaC2O 4
For example, a dog consistently fed a diet high in oxalates, such as spinach or sweet potatoes, is at a higher risk of developing calcium oxalate crystals. If this dog also has a genetic predisposition or a history of urinary tract issues, the risk is even greater. This emphasizes the importance of considering a dog’s individual risk factors when formulating a diet.
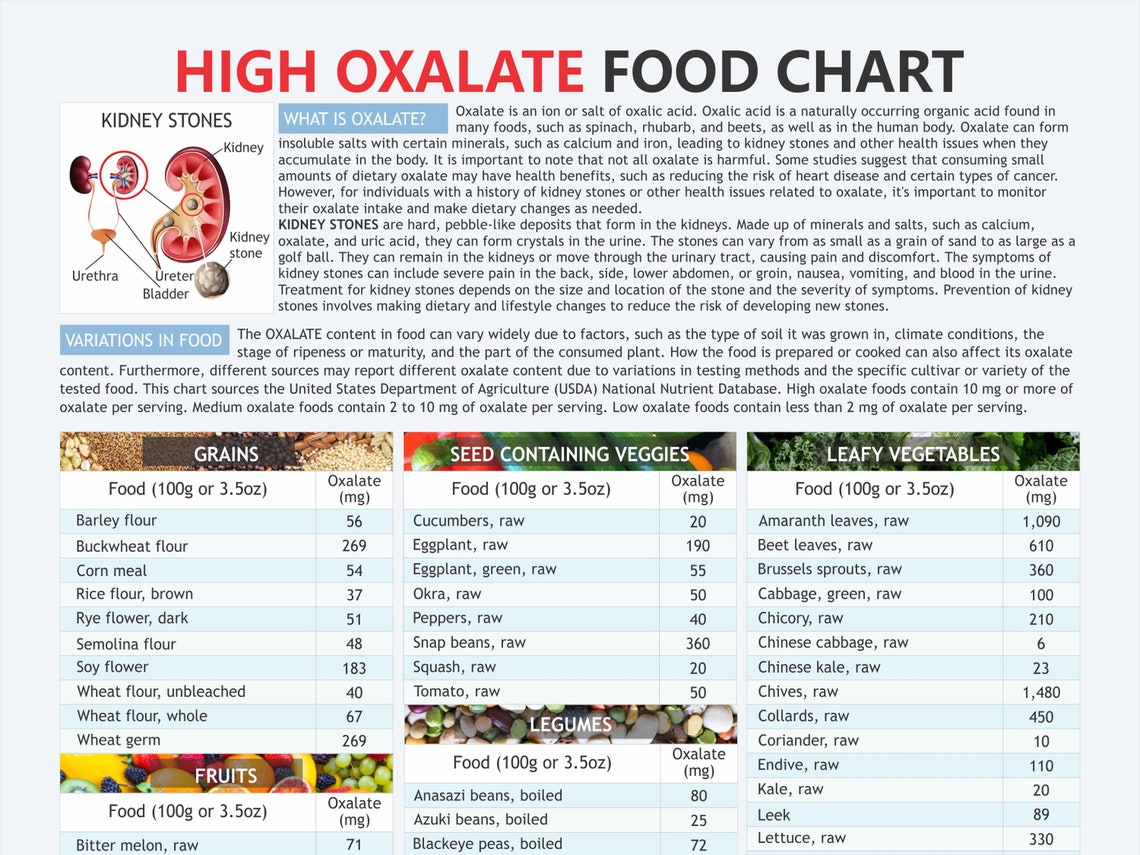
Identifying Foods High in Oxalates
Understanding which foods contain high levels of oxalates is crucial for managing a dog’s diet and potentially preventing oxalate-related health issues. This section will delve into common food items and their oxalate content, providing a clear guide for pet owners.
High-Oxalate Ingredients in Dog Food and Treats, Low oxalate foods for dogs
Many commercially available dog foods and treats contain ingredients that are high in oxalates. Awareness of these ingredients allows for more informed choices when selecting products for your dog.
- Sweet Potatoes: Often used as a carbohydrate source in dog food and treats, sweet potatoes can contain moderate levels of oxalates.
- Spinach: A common ingredient in some dog food formulations, spinach is known for its high oxalate content.
- Beets: Beetroot and beet pulp, sometimes included for their fiber content or coloring, are also high in oxalates.
- Wheat Bran: Found in some dog food formulas as a source of fiber, wheat bran can contribute to oxalate intake.
- Certain Nuts and Seeds: While less common in dog food, ingredients like peanuts and flaxseed, found in some treats or homemade recipes, can be high in oxalates.
- Chocolate: A strict no-no for dogs, chocolate is extremely high in oxalates and also contains theobromine, which is toxic to dogs.
Oxalate Content in Fruits and Vegetables
The oxalate content of fruits and vegetables varies significantly. Choosing low-oxalate options can help manage a dog’s oxalate intake. The following table provides a comparison of oxalate levels in common fruits and vegetables suitable for dogs.
| Food | Oxalate Content (mg/100g) | Notes | Alternatives |
|---|---|---|---|
| Spinach | 600-750 | Very high in oxalates. Should be avoided or given in extremely small amounts. | Kale (in moderation), Romaine Lettuce |
| Beets | 300-500 | High in oxalates. Use sparingly, if at all. | Carrots, Green Beans |
| Sweet Potato | 50-100 | Moderate oxalate content. Can be given in moderation. | Pumpkin, Butternut Squash |
| Carrots | 10-20 | Low oxalate content. A good choice for dogs. | Celery, Cucumber |
| Green Beans | 5-10 | Very low in oxalates. A safe and healthy option. | Zucchini, Broccoli (in moderation) |
| Blueberries | 10-15 | Relatively low oxalate content. A good source of antioxidants. | Raspberries, Strawberries |
| Cranberries | 80-100 | High in oxalates. Should be avoided. | Blueberries (in moderation) |
| Avocado | 0-5 | Very low oxalate content, but high in fat. Use in moderation. | Cucumber, Celery |
Impact of Cooking Methods on Oxalate Levels
Cooking methods can influence the oxalate content of foods. Certain techniques can reduce oxalate levels, offering another strategy for managing a dog’s oxalate intake.
Boiling is generally effective at reducing oxalate levels, as some of the oxalates leach into the cooking water. Discarding the cooking water is important to avoid reintroducing the oxalates.
Steaming can also help reduce oxalate content, though potentially to a lesser extent than boiling. The extent of reduction depends on the specific food and the steaming time.
Roasting and grilling typically do not significantly reduce oxalate levels. In fact, they might concentrate oxalates if the food loses moisture.
Soaking vegetables in water before cooking, especially for a longer period, can also help to leach out some oxalates. The soaking water should be discarded.
It is important to note that the effectiveness of these methods can vary based on the food and the specific cooking process used.
Introducing Low Oxalate Food Options for Dogs
Choosing the right diet for a dog with oxalate sensitivities is crucial for managing their health and well-being. This section focuses on providing practical guidance on incorporating low-oxalate food choices into your dog’s diet. We’ll explore both fresh food options and commercially available alternatives, ensuring you have the knowledge to make informed decisions about your canine companion’s meals.
Safe, Low-Oxalate Food Choices for Dogs
Selecting appropriate food items is paramount for managing oxalate levels. The following list provides a selection of safe, low-oxalate food choices suitable for dogs. Remember to always introduce new foods gradually and consult with your veterinarian to determine the best options for your dog’s individual needs.
- Proteins: Chicken, turkey, lamb, and most fish (e.g., salmon, cod) are generally low in oxalates. Eggs are also a good choice.
- Grains/Starches: White rice, cooked oatmeal, and quinoa are considered low-oxalate options.
- Vegetables:
- Cauliflower, carrots, and zucchini are generally safe.
- Green beans (in moderation) are often tolerated.
- Avoid high-oxalate vegetables like spinach, sweet potatoes, and beets.
- Fruits:
- Blueberries (in moderation) and peeled apples can be included.
- Avoid high-oxalate fruits such as raspberries and star fruit.
- Commercially Available Options: Look for dog food formulas specifically designed for urinary health or those with a low-oxalate profile. Check the ingredient list carefully and consult with your veterinarian for recommendations.
Comparing Protein Sources: Oxalate Content and Suitability
Protein sources vary significantly in their oxalate content. Understanding these differences is essential when crafting a low-oxalate diet. The following table compares common protein options, highlighting their oxalate levels and suitability for dogs with oxalate sensitivities. This information helps you make informed choices based on your dog’s specific dietary needs.
| Protein Source | Oxalate Content (Approximate) | Suitability for Dogs with Oxalate Sensitivity |
|---|---|---|
| Chicken | Low | Generally Suitable |
| Turkey | Low | Generally Suitable |
| Lamb | Low | Generally Suitable |
| Salmon | Low | Generally Suitable |
| Beef | Moderate | Use in moderation; monitor tolerance |
| Pork | Moderate | Use in moderation; monitor tolerance |
| Eggs | Low | Generally Suitable |
Importance of a Balanced Diet in Low Oxalate Food Plans
While focusing on low-oxalate foods is critical, maintaining a balanced diet remains paramount. A balanced diet provides essential nutrients to support overall health and well-being. This means incorporating a variety of ingredients within the low-oxalate guidelines.
A balanced diet should include:
- Protein: Adequate protein intake is essential for muscle maintenance and repair.
- Carbohydrates: Provide energy. Opt for low-oxalate options like white rice or oatmeal.
- Fats: Essential for energy, nutrient absorption, and overall health. Choose healthy fat sources.
- Vitamins and Minerals: Supplement as needed to ensure a complete and balanced diet, as advised by a veterinarian.
Example: A balanced meal might consist of cooked chicken (protein), white rice (carbohydrate), and carrots (vegetable). The exact proportions will vary depending on your dog’s size, age, and activity level, so always consult with your veterinarian or a veterinary nutritionist.
Commercial Dog Food Considerations
Navigating the world of commercial dog food can be complex, especially when considering a low-oxalate diet. Numerous brands and formulations exist, making it crucial to understand how to select the most appropriate option for your canine companion. This section will delve into comparing commercial dog food brands, interpreting ingredient labels, and the vital role of veterinary consultation in making informed dietary decisions.
Obtain a comprehensive document about the application of pickerington food pantry that is effective.
Comparing Commercial Dog Food Brands
Evaluating commercial dog food requires a careful examination of ingredients and potential oxalate content. Direct oxalate measurements are often unavailable from manufacturers, so assessing the likelihood of high oxalate levels relies on analyzing ingredient lists. Some brands may offer formulations specifically designed for dogs with sensitivities or specific dietary needs, which can be a good starting point. However, it’s important to thoroughly research and compare these options.For instance, consider two hypothetical dog food brands, “Healthy Hound” and “Canine Choice”.* Healthy Hound: This brand primarily uses chicken and rice as its primary protein and carbohydrate sources.
It includes ingredients like sweet potatoes and spinach, which are moderate to high in oxalates.
Canine Choice
This brand features lamb and barley as primary ingredients. It also includes a small amount of carrots and peas, which are generally considered low in oxalates.Based on this limited information, “Canine Choice” might be a more suitable option for dogs needing a low-oxalate diet due to its lower oxalate ingredients profile. However, further analysis of the complete ingredient list and brand reputation is necessary.
Reading Dog Food Labels
Understanding dog food labels is essential for identifying potential high-oxalate ingredients. The ingredient list, listed in descending order by weight, provides crucial information. Certain ingredients are more likely to contribute to oxalate intake.* High-Oxalate Ingredients: Spinach, sweet potatoes, beet pulp, and certain types of bran are examples of ingredients to be cautious about.
Moderate-Oxalate Ingredients
Carrots, peas, and potatoes can contribute to oxalate intake. Their inclusion requires careful consideration based on the overall diet.
Low-Oxalate Ingredients
Meats (chicken, lamb, beef), rice, and barley are generally considered lower in oxalates.The presence and quantity of these ingredients, as well as the overall formulation of the food, will help determine the oxalate content. Always look for the ingredient list and analyze the sources of protein and carbohydrates. Consider the use of added vitamins and minerals and their sources, as some may be derived from oxalate-rich plants.
Consulting with a Veterinarian
Before making any significant changes to your dog’s diet, consulting with a veterinarian is paramount. A veterinarian can assess your dog’s individual needs, medical history, and any existing health conditions that might be relevant to dietary choices. They can also provide guidance on the best commercial food options or whether a home-prepared diet is more suitable.Questions to ask your veterinarian:* Is a low-oxalate diet appropriate for my dog’s specific health condition?
- What are the recommended daily caloric needs for my dog, considering their age, weight, and activity level?
- Which commercial dog food brands are recommended for a low-oxalate diet, and why?
- What are the potential risks and benefits of switching to a new diet?
- How can I monitor my dog for any adverse reactions or changes after the diet switch?
- Are there any specific supplements that would be beneficial for my dog in conjunction with a low-oxalate diet?
- Can you provide guidance on how to transition my dog to a new food gradually?
- How often should I schedule follow-up appointments to assess my dog’s progress?
- What are the signs of oxalate-related health issues, and when should I seek immediate veterinary care?
- What are the potential benefits of adding certain foods to my dog’s diet to address nutritional needs?
Supplements and Support for Oxalate Management: Low Oxalate Foods For Dogs
Managing oxalate levels in dogs often necessitates a multi-faceted approach, with dietary modifications being the cornerstone. Alongside a low-oxalate diet, certain supplements may offer additional support in managing oxalate levels and mitigating potential health risks. It’s crucial to consult with a veterinarian before introducing any supplements to ensure they are appropriate for your dog’s individual needs and health status.
Calcium Citrate Supplementation
Calcium citrate is a commonly recommended supplement for dogs with oxalate-related concerns. The rationale behind its use is that calcium can bind with oxalates in the digestive tract, preventing their absorption into the bloodstream and, consequently, reducing the risk of oxalate crystal formation in the kidneys and urinary tract.
Dosage guidelines for calcium citrate supplementation vary depending on the dog’s size, weight, and the severity of the oxalate-related concerns. However, a general guideline, as suggested by veterinary nutritionists, is:
- Small dogs (under 20 lbs): 250-500 mg of calcium citrate per day, divided into two doses, given with meals.
- Medium dogs (20-50 lbs): 500-1000 mg of calcium citrate per day, divided into two doses, given with meals.
- Large dogs (over 50 lbs): 1000-2000 mg of calcium citrate per day, divided into two doses, given with meals.
The potential benefits of calcium citrate include:
- Reduced oxalate absorption in the gut.
- Decreased risk of calcium oxalate crystal formation.
- Support for overall urinary tract health.
However, potential risks associated with calcium citrate supplementation include:
- Gastrointestinal upset (e.g., constipation, diarrhea) in some dogs.
- Potential for hypercalcemia (elevated blood calcium levels), especially with excessive dosing. This is more likely in dogs with pre-existing kidney problems.
- Interference with the absorption of other minerals.
Therefore, regular monitoring of calcium levels, especially in dogs with kidney issues, is crucial. Your veterinarian can perform blood tests to monitor calcium levels and adjust the dosage as needed. A careful balance is necessary to maximize benefits while minimizing risks.
Potassium Citrate Supplementation
Potassium citrate is another supplement that may be beneficial for dogs with oxalate-related issues. Its primary role is to increase urine pH, making the urine less acidic. This creates a less favorable environment for the formation of calcium oxalate crystals.
Dosage recommendations for potassium citrate vary based on the dog’s size and urine pH levels. A veterinarian should determine the appropriate dosage through urine analysis and monitoring. However, a general starting point is:
- Small dogs: 1/8 to 1/4 teaspoon (approximately 250-500 mg) of potassium citrate, twice daily, mixed with food.
- Medium dogs: 1/4 to 1/2 teaspoon (approximately 500-1000 mg) of potassium citrate, twice daily, mixed with food.
- Large dogs: 1/2 to 1 teaspoon (approximately 1000-2000 mg) of potassium citrate, twice daily, mixed with food.
The potential benefits of potassium citrate supplementation include:
- Increased urine pH.
- Reduced risk of calcium oxalate crystal formation.
- Potential support for kidney health.
Potential risks of potassium citrate supplementation include:
- Gastrointestinal upset.
- Hyperkalemia (elevated blood potassium levels), which can be life-threatening, especially in dogs with kidney disease or those taking certain medications.
- Changes in electrolyte balance.
Regular monitoring of urine pH and electrolyte levels by a veterinarian is essential when using potassium citrate. The goal is to maintain a urine pH in the optimal range (typically between 6.5 and 7.5) to prevent crystal formation without causing excessive alkalinity.
Chitosan Supplementation
Chitosan, derived from chitin (found in crustacean shells), has been investigated for its potential to bind oxalates in the digestive tract. By binding oxalates, chitosan can help reduce their absorption and potentially lower the risk of oxalate-related problems.
Dosage recommendations for chitosan vary, but are generally based on the dog’s weight. Always follow your veterinarian’s specific instructions. A general guideline might be:
- Small dogs: 100-250 mg of chitosan, twice daily, given with meals.
- Medium dogs: 250-500 mg of chitosan, twice daily, given with meals.
- Large dogs: 500-1000 mg of chitosan, twice daily, given with meals.
Potential benefits of chitosan supplementation include:
- Reduced oxalate absorption in the gut.
- Potential support for kidney health.
Potential risks of chitosan supplementation include:
- Gastrointestinal upset.
- Interference with the absorption of fat-soluble vitamins (A, D, E, and K).
Chitosan should be administered separately from other medications or supplements to minimize potential interactions. Monitoring for any signs of digestive upset or vitamin deficiencies is important.
Vitamin B6 Supplementation
Vitamin B6 (pyridoxine) plays a crucial role in oxalate metabolism. Some studies suggest that it can help reduce the formation of oxalates in the body.
Dosage recommendations for Vitamin B6 supplementation vary. Always consult with your veterinarian for appropriate dosage. General guidelines might be:
- Small dogs: 1-5 mg of Vitamin B6 per day.
- Medium dogs: 5-10 mg of Vitamin B6 per day.
- Large dogs: 10-25 mg of Vitamin B6 per day.
Potential benefits of Vitamin B6 supplementation include:
- Reduced oxalate production in the body.
- Potential support for kidney health.
Potential risks of Vitamin B6 supplementation include:
- Generally considered safe at recommended dosages.
- High doses may lead to neurological issues.
It’s essential to follow your veterinarian’s dosage recommendations closely and monitor for any adverse effects. Over-supplementation can lead to adverse health issues.
Other Supportive Measures
In addition to the supplements mentioned above, other supportive measures can be beneficial in managing oxalate levels and promoting overall health in dogs.
- Adequate Hydration: Ensuring your dog has access to fresh, clean water at all times is crucial. Proper hydration helps to flush the urinary tract and dilute urine, reducing the risk of crystal formation.
- Regular Exercise: Encouraging regular physical activity promotes overall health and can help with kidney function.
- Frequent Veterinary Checkups: Regular veterinary checkups, including urine analysis and blood tests, are essential for monitoring kidney function, urine pH, and electrolyte levels. These tests help assess the effectiveness of the treatment plan and identify any potential complications.
Monitoring and Management of Oxalate Issues
Maintaining a low-oxalate diet for your dog requires ongoing vigilance and proactive management. This section focuses on how to monitor your dog’s health, recognize potential problems related to oxalate accumulation, and implement strategies to address and mitigate these issues. Early detection and consistent management are crucial for ensuring your dog’s long-term well-being.
Regular Check-ups and Testing
Consistent monitoring is essential to assess the effectiveness of a low-oxalate diet and to detect any emerging health concerns. This involves regular veterinary check-ups and specific diagnostic tests.Veterinary check-ups should be conducted at least annually, or more frequently as recommended by your veterinarian, especially if your dog has a history of oxalate-related issues. These check-ups typically include:
- Physical Examination: A thorough examination to assess overall health, including hydration, body condition, and any signs of discomfort.
- Urinalysis: A urine sample is analyzed to assess urine concentration, pH, and the presence of crystals, such as calcium oxalate crystals. The presence of these crystals is a key indicator of oxalate issues.
- Blood Work: Complete blood counts (CBC) and chemistry panels are performed to evaluate kidney function (BUN, creatinine), electrolyte balance, and overall organ health.
- Imaging (if necessary): X-rays or ultrasounds may be recommended to visualize the kidneys and bladder, and to detect any stones or abnormalities.
Specific tests to monitor oxalate levels may include:
- Urine Oxalate Measurement: This test directly measures the amount of oxalate excreted in the urine. Elevated levels can indicate a problem.
- Kidney Function Tests: BUN (blood urea nitrogen) and creatinine levels are crucial indicators of kidney health. Increased levels suggest potential kidney damage.
Regular monitoring allows for early detection of problems and prompt intervention. For example, a dog with a history of calcium oxalate uroliths might require more frequent urinalysis, perhaps every 3-6 months, to monitor for recurrence.
Recognizing Signs of Oxalate-Related Health Problems
Being able to recognize the signs of oxalate-related health problems in dogs is crucial for timely intervention. These signs can vary depending on the location and severity of the issue.Common signs include:
- Urinary Issues:
- Difficulty urinating: Straining to urinate or inability to urinate at all.
- Frequent urination: Increased frequency of urination, even if only small amounts are produced.
- Blood in urine (hematuria): Urine may appear pink, red, or contain blood clots.
- Incontinence: Loss of bladder control.
- Changes in Drinking and Appetite:
- Increased thirst (polydipsia): Drinking more water than usual.
- Decreased appetite (anorexia): Loss of interest in food.
- Vomiting: Episodes of vomiting, potentially due to kidney issues or pain.
- Lethargy and Weakness:
- General weakness: Reduced activity level.
- Lethargy: Excessive tiredness or lack of energy.
- Abdominal Pain:
- Painful abdomen: Dog may show signs of discomfort when the abdomen is touched.
- Restlessness: Inability to settle comfortably.
Early detection of these signs is vital. For example, a dog exhibiting frequent urination and straining may have a urinary tract obstruction due to oxalate stones, requiring immediate veterinary attention.
Strategies for Managing Oxalate Issues
Managing oxalate issues in dogs involves a multi-faceted approach that includes dietary adjustments, medical interventions, and ongoing monitoring. The specific strategies employed will depend on the severity of the problem and the individual dog’s needs.Dietary adjustments form the cornerstone of oxalate management:
- Strict Adherence to a Low-Oxalate Diet: This involves carefully selecting commercially available dog foods or preparing homemade meals that are low in oxalate. Review the ‘Introducing Low Oxalate Food Options for Dogs’ section.
- Adequate Water Intake: Ensuring the dog drinks plenty of water helps to dilute urine and reduce the concentration of oxalate. Fresh water should always be available.
- Controlled Mineral Intake: In some cases, the veterinarian may recommend adjusting the levels of minerals such as calcium and phosphorus in the diet to minimize the risk of stone formation.
Medical interventions may be necessary, depending on the severity of the condition:
- Medications:
- Potassium citrate: This medication can help alkalinize the urine, which may prevent the formation of calcium oxalate crystals.
- Diuretics: In some cases, diuretics may be prescribed to increase urine production and flush out oxalate crystals.
- Pain medication: To manage pain associated with stone formation or urinary tract infections.
- Stone Removal:
- Medical dissolution: In some cases, stones can be dissolved with specific medications.
- Surgery: Surgical removal of stones may be necessary if they are too large or causing obstruction.
- Lithotripsy: A procedure using shock waves to break up stones into smaller fragments.
- Treatment of Underlying Conditions: If an underlying condition, such as a metabolic disorder, contributes to oxalate issues, it must be addressed.
Ongoing monitoring is critical to evaluate the effectiveness of management strategies. Regular check-ups, urinalysis, and blood work should be performed to monitor the dog’s condition and make necessary adjustments to the treatment plan. For example, a dog that has undergone surgery to remove oxalate stones may require lifelong dietary management and periodic check-ups to prevent recurrence.
Ending Remarks
In conclusion, managing your dog’s oxalate intake through careful food selection and dietary adjustments is a proactive approach to ensuring their long-term health. This guide has equipped you with the necessary tools to navigate the world of low oxalate foods, empowering you to make informed choices that promote your dog’s well-being. Remember to always consult with your veterinarian for personalized advice.


